Exploring the Power of PEA for Pain Management
PEA is a natural substance produced by our body. It is our in built pain modulator that works via our ‘bliss’ receptors.
The benefits of PEA as a natural anti-inflammatory agent was first identified in the 1950’s (4). Also found in eggs, cow’s milk, breast milk, beans, peas, tomato, alfalfa, corn, soy beans (2) it has only been recently that it has gained attention for use in pain management.
PEA: A novel anti-neuroinflammatory compound
Nobel Prize winner Levi-Montalcini identified PEA or palmitoylethanolamide as a naturally occurring molecule, describing its value in treating chronic infections and pains. Following her discovery, hundreds of scientific studies have been carried out to show that it is very effective and safe to use.
PEA is an endogenously produced cannabimimetic compound (1) with analgesic, anti-inflammatory and neuroprotective effects. (2) PEA is found everywhere in our bodies, as is produced on demand from the lipid bilayer. (4) PEA belongs to a group of bioactive lipids called N-acylethanolamines (NAEs) which are involved in the regulation of pain and inflammation. It is particularly abundant in the central nervous system (CNS), where it is produced by neurons and glial cells, and also in immune cells.(5)
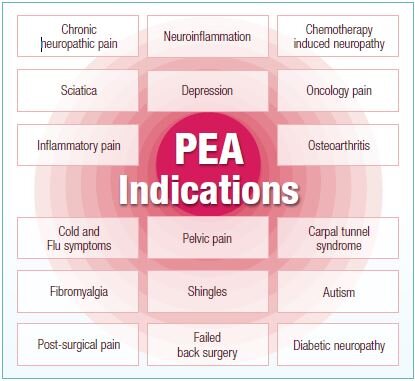
PEA Indications
What is PEA indicated for?
Often in people with chronic disorders, the body does not produce enough PEA, which causes problems. Taking PEA to supplement the body’s shortage may be beneficial if you have neuropathic pain, inflammatory pain and/or a neuro-inflammatory condition.
Neuropathic Pain
Neuropathic pain, caused by the damage or dysfunction of nerves, is often experienced as shooting, radiating, tingling, stabbing or burning pain. The compression of nerves, as found in sciatica or carpal tunnel syndrome, is a common cause of neuropathic pain. Other common causes include post-herpetic neuralgia (shingles), persistent post surgical pain, diabetic neuropathy, pelvic pain, sciatic pain, fibromyalgia and complex regional pain syndrome.18,19
What is neuropathic pain?
Neuropathic pain is one of the most difficult chronic pain conditions to treat. The dynamic nature of the nervous system means that changes to its structure — for example damage caused by long term compression or inflammation of the nerves – allow the nerves to continue to send pain signals to the brain long after the original cause of the pressure on the nerves has been removed.
This “pain memory” can lead to “pain sensitisation” where the threshold of pain receptors to stimuli is reduced, allowing even light touch of the affected area to induce the sensation of pain.19 The compression of nerves induces inflammation within the nerve and nerve root; this is largely mediated by inflammatory cells which results in nerve sensitisation. Microglia in the CNS may then be activated, propagating neuro-inflammation through the recruitment of other microglia and astrocytes, thereby leading to chronic pain.20
PEA’s ability to inhibit mast cell migration and activation, and the over-activation of glia and astrocytes, has led to it being extensively studied in neuropathic pain, where it is particularly effective in trapped nerve pain such as sciatica and carpal tunnel syndrome, as well as chronic pelvic pain, arthritis of the TMJ, and pain from radiculopathy.
-
A 2015 review of eight published clinical trials on the use of PEA in nerve entrapment syndromes in 1366 patients found PEA to be effective and safe in these conditions.13
-
It has been shown that 26% of pain from knee osteoarthritis is neuropathic.24
-
More than 50% of diabetic patients have some degree of peripheral neuropathy.
-
Chemotherapy-Induced peripheral neuropathy (CIPN) is a common side effect of chemotherapy and occurs in as many as 68% of patients within the first month of chemotherapy treatment.
Inflammatory Pain: Fibromyalgia
Fibromyalgia is a common condition affecting 2–5% of the population and is primarily seen in young and middle-aged women. It is characterised by widespread musculoskeletal pain and tenderness, poor quality sleep and significant fatigue, in addition to cognitive disturbances including poor concentration and memory, and high levels of distress.
The underlying pathophysiology involves the development of “central sensitisation” changes in the CNS which result in usually non-painful stimuli being experienced as painful. (30)
A clinical trial in 35 patients who had undergone standard treatment with duloxetine and pregabalin for three months demonstrated that the addition of PEA to standard treatment for an additional three months (600mg bd for one month, then 300mg bd for two months) significantly improved VAS ratings from 3.7 to 1.9 (p<0.0001), and significantly reduced the number of Tender Points (p<0.0001).31
Neuro-Inflammatory Conditions: Depression
Emerging data demonstrates that the pathogenesis of major depression involves immuno-inflammatory markers including interleukin (IL)-1, IL-6 and TNF-α. Impairment of endocannabinoid signalling is also implicated in mood disturbances and other neuropsychiatric disorders. Due to PEA’s anti-inflammatory and neuroprotective effects and its influence on cannabinoid receptor expression, it has been proposed as a beneficial adjunct to the treatment of depression.32
PEA is not a Panacea
It is well recognised that any chronic pain condition is best addressed within a person centred and whole systems approach. As such, the prescription of PEA is best given as part of a broad treatment protocol which addresses all factors contributing to a persons pain experience.
Examples of Co-prescriptions considered by a Naturopath
Inflammatory pain – fish oils,magnesium, bioflavonoids and herbal mediciens such as Salix alba and Curcuma longa
Neuropathic Pain – B vitamins, NAC and various herbal medicines
Neuro-inflammatory conditions – Probiotics, Gingko biloba, Hypericum perforatum
Other treatment protocols are considered for factors such as sleep quality, anxiety, depression, inflammation, diet and lifestyle.
Safety and Dosing
The daily dosage of PEA in clinical trials has ranged from 300 mg–1200 mg daily for chronic pain. Individual requirements will vary and some can take up to 4 -6 weeks to experience benefits. PEA is available powder, capsule or liquid form.
Considering that PEA is a fat soluble compound, consumption with a fat-containing meal may enhance absorption. PEA has been clinically studied across a broad population group and has been found to be highly tolerable. There are no known side effects abut my experience has been that some people do however have digestive disturbance. This can be addressed by dosing correctly.
PEA can be taken together with any other substance. It enhances the pain-relieving effect of classic analgesics and anti-inflammatories.
Written by Sasha Wray
Practice Principal Occupational Therapist, Naturopath and 5 Element Acupressure Practitioner
This blog has been adapted from Practitioner information provided by Biomedica
Copyright Next Wave Therapy