Hundreds of Headaches
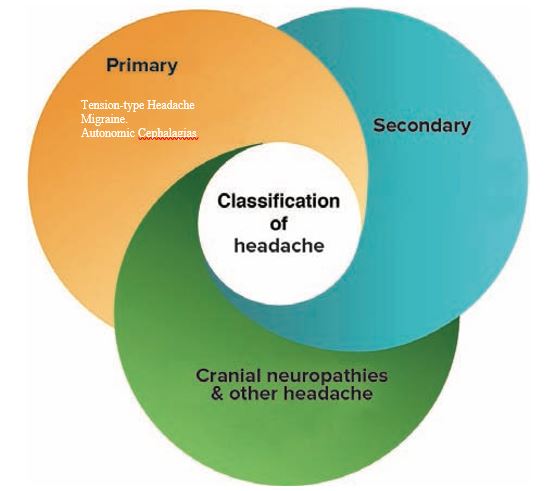
Headache is one of the most prevalent pain conditions in the global population affecting people at all stages of life (1). There are literally hundreds of different forms of headaches, which are broadly classified into 3 main categories by the International Headache Society (IHS) (2).
If you’re someone who experiences headaches you don’t need to be reminded of how much it affects your everyday life. In this blog, Jonathan Wray (Principal Physiotherapist at Next Wave Therapy) gives a clear overview of the different types of headache, highlighting both the importance and difficulty of accurate diagnosis and giving some guidelines for evidenced based treatment options.
The three main categories of headache are:
-
Primary headaches; migraine, tension type headache and trigeminal autonomic cephalagias (e.g. cluster headaches)
-
Secondary headaches; Cervicogenic (originating from the upper neck and base of skull), Vasuclar, Medication overuse, Infection induced.
-
Cranial neuropathies; Lesions of the cranial nerves.
Figure 1. Adapted From Bukner and Khan, Clinical Sports Medicine 2017 (1)
Most common types of headache
The most common type of headache is tension type headache with a global prevalence of 38%, then migraine 10%, and lastly chronic daily headache 3% and cervicogenic headache 2.5-4% (3). Effective treatment of these headaches relies on good diagnosis and classification.
The difficulty for headache sufferers is that they often experience more than one type of headache. Therefore unless they receive a thorough assessment through in-depth questioning about their symptoms and a targeted physical examination, treatment can often be mis-matched and ineffective.
Each headache type has specific diagnostic criteria therefore it is crucial for headache sufferers to seek a suitably experienced health care provider.
At Next Wave Therapy in Hilton (Fremantle area) we usually see the 3 common types of headache. These are the tension type headache, cervicogenic and migraine. It is also not uncommon for a tension type headache or cervicogenic headache to trigger a migraine. This further supports the need for a targeted and thorough assessment.
Tension Type Headaches
Diagnostic criteria:
-
A – At least 10 episodes of headache occurring on <1 day/month on average (<12 days/year) and fulfilling criteria B–D.
-
B – Lasting from 30 minutes to seven days.
-
C – at least 2 of the following 4 characteristics; bilateral location, pressing or tightening (non pulsating), mild or moderate intensity, not aggravated by routing physical activity.
-
D – Both of the following; no nausea or vomiting, only one of phono or photophobia.
The exact mechanisms responsible for tension type headaches are not fully understood. Altered peripheral sensory processing is thought to play a role and altered sensory processing in the brain stem. More persistent or chronic presentations are associated with increased tenderness of muscles around the face neck and jaw.
Treatment Options
Tension type headache can respond well to over the counter medication such as Aspirin, Ibuprofen and other non-steroidal anti-inflammatory medication (4) however they will not respond to medication commonly used for migraines such as Triptans. However classification of headaches between tension type headache and migraine often causes a dilemma as distinguishing between a tension type headache and a milder forms migraine without aura can be challenging especially as headache sufferers can experience both.
More strict diagnostic criteria have been suggested but this has only really helped to classify headaches as “probably” tension type headache or “probably” migraine. There is some good evidence for the use of tri-cyclic antidepressants in preventing tension type headache (4).
Non-pharmacological management of tension type headache as well as migraine is often to identify common triggers e.g. postural, movement, food or activity based. Maintaining a healthy lifestyle through adequate exercise, adequate hydration and by eating regular meals. Positive responses to prevention of headaches using Mindfulness Based Stress Reduction, Act and Commitment Therapy (ACT) and meditation have been observed and this is an increasing area of research (5).
Cervicogenic Headache
Diagnostic Criteria
-
Unilateral headache without side shift
-
Neck pain on same side, shoulder and arm pain of a rather vague, non-radicular nature.
-
Pain episodes of varying duration or fluctuating, continuous pain
-
Moderate, non-excruciating pain, usually of a non-throbbing nature
-
Pain starting in the neck, eventually spreading to head, where the maximum pain is often located
-
Pain triggered by neck movement and/or sustained awkward position
-
Sustained neck trauma prior to the onset
-
Autonomic symptoms and signs (e.g. nausea, vomiting, dizziness, photo- and phonophobia, blurred vision)
-
Reduced cervical spine range of motion
-
Symptoms on palpation of the cranium or neck
-
Anaesthetic blockades abolish the pain transiently
Cervicogenic headache is a common secondary type of headache that we see at Next Wave. This is a secondary headache as its origin is usually from the upper part of the neck. The information coming into the brain from the structures in this part of the neck converge in part of the mid brain with information coming from other parts of the face and head. The processing of this converging information can lead to the feeling that the pain is referring to the head and face (6). Key features in this headache presentation are that pain starts in the neck and refers to head / face, there is a restriction of movement in the upper neck and that reproduction of symptoms can be reproduce d by palpation of structures in the upper neck. Common issues found in people with cervicogenic headache are less than optimal control of the neck and shoulder musculature which inadvertently adds unnecessary loads to the upper part of the neck.
Treatment Options
There is good evidence for treatment to consist of manual therapy, exercise and postural re-education (1). Physiotherapy has a significant role to play in helping to improve the lives of people who experience this type of headache.
Migraine (without aura)
A migraine generally lasts between 4 and 72 hours. Usually unilateral (one sided), moderate to severe intensity, pulsating quality and associated phono or photophobia (sensitivity to sound or light).
Underlying cause of migraine without aura was previously thought to be primarily vascular but more recent research has also included sensitization of the nervous system as a contributing factor. Sensory information entering the brain is not modulated in a normal way and therefore can be interpreted as pain due to this altered processing. It is now clear that migraine without aura is a neurobiological disorder (1) (2).
Diagnostic criteria
-
5 Headaches that satisfy that satisfy the following criteria.
-
Lasts 4-72 hours if untreated or unsuccessfully treated
-
Has at least 2 of the following 4 characteristics – unilateral, Pulsating, moderate to severe, aggravated or avoidance of routing physical activity.
-
During the headache at least 1 of the following – nausea +/- vomiting, phono/photophobia
Migraine with Aura
Recurrent attacks, lasting minutes, of unilateral fully reversible visual, sensory or other central nervous system symptoms that usually develop gradually and are usually followed by headache and associated migraine symptoms.
Diagnostic criteria
At lease 2 attacks fulfilling criteria B and C
B. One or more of fully reversible aura symptoms:
-
Visual
-
Sensory
-
Speech / language
-
Motor
-
Brainstem
Retinal
C. At least 3 of the following 6 characteristics
-
At least 1 aura symptom spreads gradually over more than 5 mins
-
2 or more aura symptoms occur in succession
-
Each individual aura lasts 5-60 mins
-
At least 1 aura symptom is unilateral
-
At least 1 aura symptom is positive
-
The aura is accompanied or followed within 60 mins by a headache.
Visual aura is the most common (90% of people) followed by sensory disturbance i.e. pins and needles moving from the point of origin and affecting one side of the body face or tongue. Less common are speech disturbances (2).
Other causes of headache
Other causes of headache that are often over looked and deemed to be secondary type headaches are substance withdrawal, medication overuse and caffeine.
Although uncommon there are also potentially more serious medical pathologies associated with headaches and if you are at all worried we suggest discussing this with you GP or other medical health professional.
Conclusion
There are hundreds of different types of headaches and some can trigger other types making it difficult to accurately diagnose which type(s) a person is experiencing. Effective treatment outcomes are seen when time is spent accurately identifying contributing factors to headache. This enable the physiotherapist to devise a targeted treatment plan with the patient.
Physiotherapy treatment offered at Next Wave may involve manual therapy, acupuncture, exercise prescription and posture re-education. Other therapies offered at Next Wave which are indicated for headache include myo-fascial massage therapy, Acceptance and Commitment Therapy and relaxation training, diet and nutritional medicine.
Next Wave offers compelling therapy to enrich everyday living.
Written by Jonathan Wray, Principal Physiotherapist. Jonathan has a special interest in treating headache, neck and upper limb disorders.
References
1. Hall T. Headache. In: Clinical Sports Medicine. McGraw Hill; 2017. p. 317–30.
2. Vincent M, Wang S. The International Classification of Headache Disorders , 3rd edition. 2018;38(1):1–211.
3. Hall T, Briffa KN, Hopper D. Hall review cgh 08. J Man Manip Ther. 1999;16(2):73–80.
4. Burch R. Migraine and Tension – Type Headache Diagnosis and Treatment. Med Clin NA [Internet]. 2018; Available from: https://doi.org/10.1016/j.mcna.2018.10.003
5. Silberstein SD, Education T. PRACTICE PARAMETER : EVIDENCE-BASED GUIDELINES FOR MIGRAINE HEADACHE ( AN EVIDENCE-BASED REVIEW ). 2000;
6. Bogduk N, Govind J. Cervicogenic headache : an assessment of the evidence on clinical diagnosis , invasive tests , and treatment. Lancet Neurol [Internet]. 2009;8(10):959–68. Available from: http://dx.doi.org/10.1016/S1474-4422(09)70209-1