Have you got pain on the outside of your hip?
People can get pain on the outside of their hip for a number of reasons. Often it’s accompanied by back pain, leg pain or pain in other areas. So a thorough physiotherapy assessment is essential to identify the underlying cause and formulate a targeted treatment plan.
What causes hip pain?
One of the most common reasons for pain on the outside of the hip or “lateral hip pain”, is due to an irritation or injury to the tendons of the gluteal muscles. This is often diagnosed on an ultrasound scan or MRI and other findings such as greater trochanteric bursitis (a small bit of cushioning under the tendon) may also be present. There are some really useful clinical tests that can be performed by a physiotherapist that give an accurate diagnosis even if you haven’t had imaging and are more helpful in discovering the source of you hip pain than scans alone (Grimaldi et al., 2015).
This common and often debilitating condition affects both sedentary and athletic adults but is more predominant in females aged over 40 years (Grimaldi et al., 2015). Activities such as sleeping on the side, walking, climbing stairs and sitting often become painful.
The good news is that this responds well to a specific exercise program and physiotherapy has been shown to be very effective in managing this condition (Mellor et al., 2016)(Mellor et al., 2018). There are also some “dos” and “don’ts”, discussed later in the blog, that help by reducing irritating or provocative positions.
Firstly lets talk a about the gluteal muscles and why they could be causing pain on the outside of your hip.
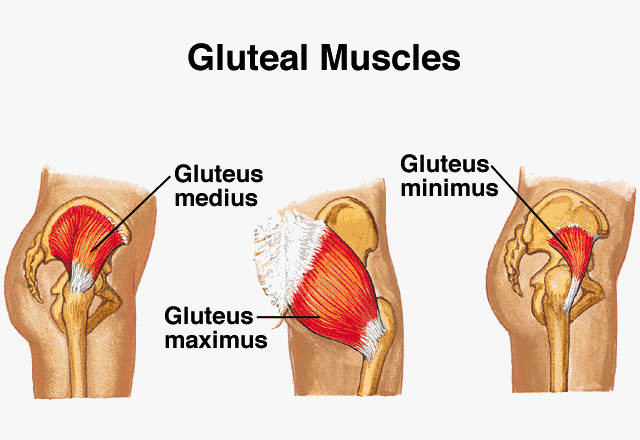
The gluteal muscles involved are Gluteus medius and Gluteus minimus. If you look at the above picture you can see that these muscles originate on the side of your pelvis and their tendons attach into a bony prominence just at the top of the outside of your thigh called the greater trochanter.
One of the main functions of these two muscles is to control the sideways movement of the pelvis on the hip during activities such as running, walking, stair climbing etc.
It is thought that the main reason these structures produce pain is because they become irritated or injured due to being overloaded with changes in activity or being compressed against the bony greater trochanter and an overlying thick band of fascia called the iliotibial band (Mellor et al., 2016)
Contributing factors in this type of presentation include:
-
Weakness of the gluteal muscles (resulting in less than optimal control of the pelvis on the lower limb)
-
Tightness of structures that run over the gluteal tendons
-
Tightness of muscles that pulls the hip into a more midline (adducted position)
-
Imbalances in activation of muscles around the hip
-
Changes in activity or demand on these muscles e.g. walking, running, lunging, jumping (Grimaldi et al., 2015).
So who do we typically see with this type of presentation in the clinic?
Well as mentioned before it is much more common in women and particularly those over 40 years old. Usually there is something in the patient’s story that leads us to suspect that it may be an irritation of the tendons such as a change in activity levels either as a one off or a decision to become more active.
Different types of activity that the body is not as accustomed to may be a trigger. And so can a sedentary lifestyle, as the muscles and tendons become deconditioned and have difficulty coping with even the normal demands of daily activity. Often it is not obvious what has caused the pain on the outside of your hip as there is not usually an obvious traumatic event. However a physiotherapy assessment will be able to diagnose the underlying issue and set you on a path to recovery and beyond.
What can you do at home to alleviate pain in your hip?
The first thing to do is to reduce the irritation so that you can let symptoms settle down and get them under control. Ice and Anti-inflammatory medication particularly Ibuprofen (as it has been shown to promote tendon cell production) can be useful for settling an acute flare up of tendon related pain (Malliaras & Purdam, 2014) so speak to your pharmacist or GP to see if this is appropriate for you. Irritated tendons will not like being overloaded or compressed as this will keep them sensitised and painful so activity modification is a must.
My top 3 tips for helping settle symptoms are to avoid positions that will add a compressive element to the outside of the hip and the sensitized tendons involved.
-
Avoid sitting with legs crossed
-
Avoid sleeping on the irritated side
-
Avoid stretching the muscles involved
(Grimaldi & Fearon, 2015)
Instead I recommend that you:
-
Sit with legs hip width apart
-
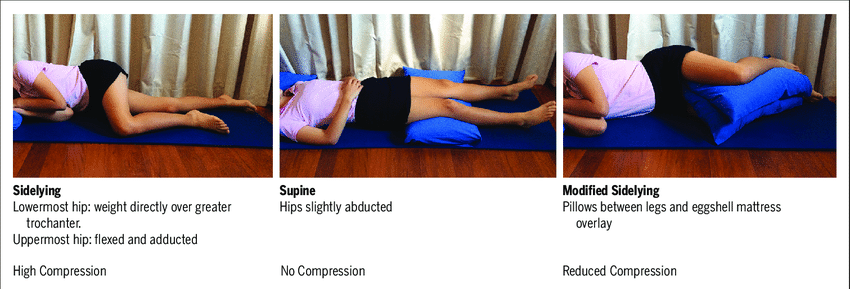
Sleep on the unaffected side with a large pillow between your legs or sleep on your back with a pillow under your knees.
-
Avoid stretching the muscles involved.
Below the picture on the left shows a side lying position to avoid. The middle picture and one on the right show less provocative sleeping positions. (Grimaldi & Fearon, 2015)
Steps to Recovery and Beyond
Specific exercises targeting the gluteal muscles involved can be started immediately and static contractions of these muscles called “isometric” contractions can have pain-relieving affects (Malliaras & Purdam, 2014). As symptoms settle you can make these muscles work harder stimulating cellular changes that will make the muscles and tendons more resilient and able to cope with increased demand without producing pain. This type of treatment plan has been shown to be very successful (Mellor et al., 2018) but it needs to be conducted and progressed appropriately over 8 to 12 weeks and ideally with the guidance of an experienced physiotherapist.
If you would like any more information on treatment approaches for hip pain feel free to contact us at Next Wave Therapy
Written by Jonathan Wray BSc (Hons) Physiotherapy, Masters Clinical Physiotherapy, Associate Fellow Australian College of Physiotherapy, Principle Physiotherapist Next Wave Therapy, Copyright © Next Wave Therapy
References
Grimaldi, A., & Fearon, A. (2015). Gluteal Tendinopathy: Integrating Pathomechanics and Clinical Features in Its Management. Journal of Orthopaedic & Sports Physical Therapy. https://doi.org/10.2519/jospt.2015.5829
Grimaldi, A., Mellor, R., Hodges, P., Bennell, K., Wajswelner, H., & Vicenzino, B. (2015). Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management. Sports Medicine, 45(8), 1107–1119. https://doi.org/10.1007/s40279-015-0336-5
Malliaras, P., & Purdam, C. (2014). Proximal hamstring tendinopathy assessment and management. Sport Health, 32(1), 21. Retrieved from http://search.informit.com.au/documentSummary;dn=322956474452988;res=IELHEA
Mellor, R., Bennell, K., Grimaldi, A., Nicolson, P., Kasza, J., Hodges, P., … Vicenzino, B. (2018). Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: Prospective, single blinded, randomised clinical trial. BMJ (Online), 361. https://doi.org/10.1136/bmj.k1662
Mellor, R., Grimaldi, A., Wajswelner, H., Hodges, P., Abbott, J. H., Bennell, K., & Vicenzino, B. (2016). Exercise and load modification versus corticosteroid injection versus “wait and see” for persistent gluteus medius/minimus tendinopathy (the LEAP trial): A protocol for a randomised clinical trial. BMC Musculoskeletal Disorders. https://doi.org/10.1186/s12891-016-1043-6