Occupational Therapy for POP
Lifting the lid on Pelvic Organ Prolapse
It is Pelvic Organ Prolapse (POP) awareness month. Because POP is one of those secretive topics related to women’s health, it is important that we raise awareness about what it is, who it affects, and how it can be managed.
POP can occur in women of all ages. About 50 percent of women who have birthed children experience pelvic organ prolapse. This means, if you are experiencing POP, you are not alone. The prolapse may occur, or first become noticeable when transitioning into menopause.
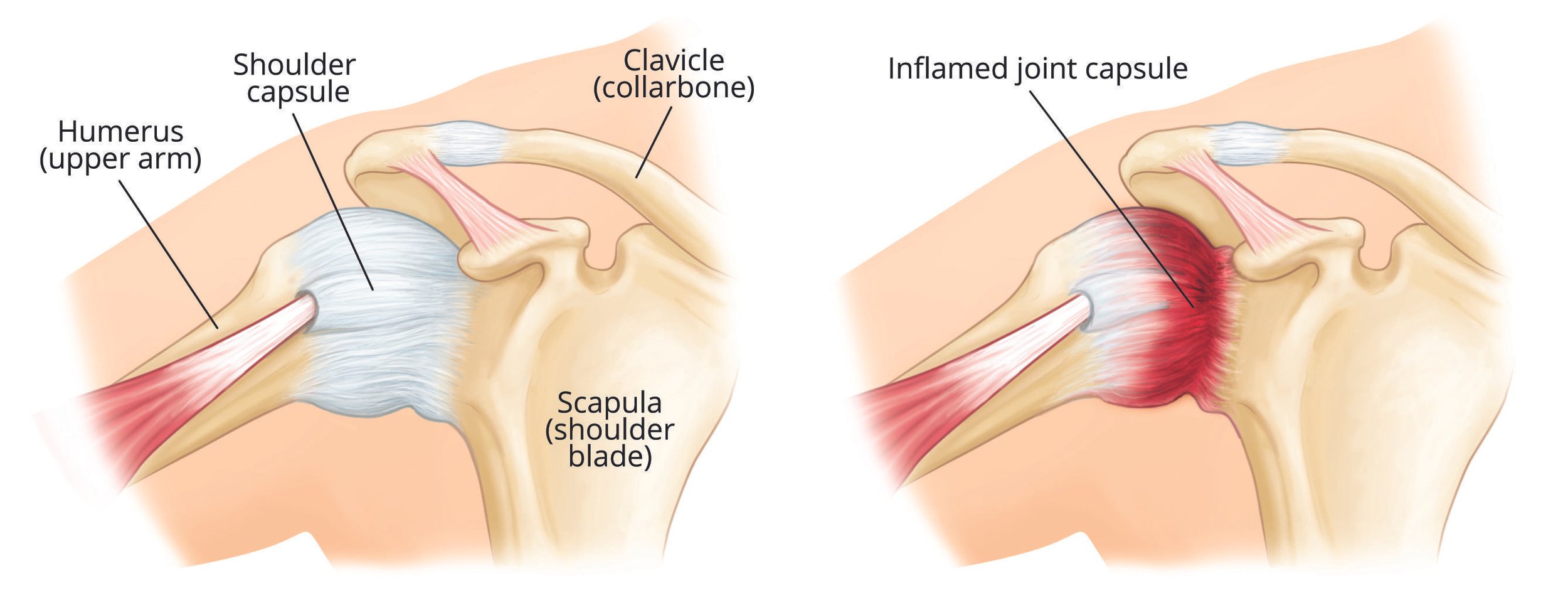
What is Pelvic Organ Prolapse?
Pelvic Organ Prolapse or POP is the descent of one or more walls of the vagina, the uterus or the cervix. This means that the structures that support these organs, have stretched. These organs are typically supported by fascia, ligaments and the pelvic floor muscles.
4 Main Types of Prolapse
- The bladder bulging into the front wall of the vagina (anterior prolapse)
- The womb bulging or hanging down into the vagina (uterine prolapse)
- The top of the vagina sagging down – this happens to some women after they have had surgery to remove their womb
- The bowel bulging forward into the back wall of the vagina (posterior wall prolapse)
It’s possible to have more than 1 of these at the same time. Pelvic organ prolapse will usually be classified on a scale of 1 to 4 to show how severe it is, with 4 being a severe prolapse.
What Causes Pelvic Organ Prolapse?
Pelvic organ prolapse happens when the group of muscles and tissues that normally support the pelvic organs, called the pelvic floor, becomes weakened and cannot hold the organs in place firmly.
A number of things can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse. These include:
- Childbirth, especially if you had a long, difficult birth, or if you gave birth to a large baby or multiple babies. Not surprisingly this is due to pressure on the pelvic floor muscles and connective tissue, strain during vaginal birth, injuries to the pelvic floor during birth. The supporting structures may also become lax, resulting in pelvic organ prolapse
- Getting older and going through menopause; age related estrogen loss which impacts muscle tissue strength, elasticity, and density, including internal muscle tissue such as the pc muscle
- Chronic Constipation – Chronic straining during bowel movements, also IBS (irritable bowel syndrome), poor diet, lack of exercise may cause constipation
- Heavy lifting including lifting children, repetitive heavy lifting at work, weight lifting
- Being overweight
- Chronic coughing; smoking, allergies, bronchitis, and emphysema may cause chronic coughing
- Having a long-term health condition that causes you to cough and strain
- Having a hysterectomy
- Abdominal surgery; structural weakness from surgery, myofascial restrictions, and scar tissue can lead to amplify POP complications.
- Diastasis rectus abdominus (DRA) muscle separation during pregnancy may predispose women to a core weakness which can increase to POP risk factor
- Some health conditions can also make a prolapse more likely, including neuromuscular diseases like Ehlers Danlos Syndrome, MS.
Symptoms of Pelvic Organ Prolapse
- Feeling like your “insides are falling out” or like you are sitting on a ball.
- Inability to keep tampon in or a sensation that tampon is slipping out
- “Heavy” or “dragging” sensation in the pelvis
- Difficulty fully emptying bowels or bladder
- Lower back pain
- Pressure, pain, or fullness in vagina, rectum, or both
- Vaginal tissue bulge
- Urinary incontinence
- Urine retention (feel urge but unable to urinate)
- Fecal incontinence
- Chronic constipation
- Back/pelvic pain
- Lack of sexual sensation
- Painful intercourse
Myths Around Pelvic Organ Prolapse
“If I have a prolapse, my uterus could fall out”
False: Although it may feel uncomfortable and as if something is going to fall out, the structures will not actually fall out.
“If you have a prolapse, you should avoid exercise”
False: You are able to build strength in your pelvic floor through all your daily movements to avoid further injury. It is a great idea to have guidance with returning to movement.
“Prolapse causes pelvic pain”
False: Although it is an uncomfortable feeling, this is not the cause of pelvic pain conditions such as vulvodynia or vaginismus.
“You have to have surgery to fix the prolapse”
False: First line treatment for POP is Pelvic floor treatment with a physiotherapist or occupational therapist. Very often this can help to heal and get back to their normal. iI surgery is needed these professionals can support you, advise and provide pre and post surgery treatment required
Can Occupational Therapy Treat Pelvic Organ Prolapse (POP)?
Yes! The good news is that there is great evidence that pelvic organ prolapse can be treated with occupational therapy.
Therapy will involve assessing the pelvic floor muscles for coordination and strength. A pelvic health occupational therapist will discuss home exercises and behavioural change.
Since the pelvic organ prolapse is directly related to intra abdominal pressure, it is important to manage this pressure during exercise and during your daily activities.
Therefore therapy may involve ergonomic assessments to ensure your posture is allowing your pelvic floor to support you during your day.
Occupational Therapy Treatment for Pelvic Organ Prolapse
If you have been diagnosed with a pelvic organ prolapse, book an initial consultation with a Women’s Health Occupational Therapist at Next Wave Therapy. Our therapists specialise in behavioural retraining, pelvic floor training and functional exercise rehabilitation.
Choosing to prioritise your pelvic health will help you to get back to the activities that you love and to feel strong while doing them.
Care plans provided by OT are unique to you and your goals. Modalities may include:
sEMG Biofeedback guided pelvic floor muscle training (neuromuscular re-education)
- Exploring behavioural, lifestyle and habit changes to support your pelvic health
- Exploring your sensory processing preferences to support your nervous system regulation
- Rehabilitative exercises
- Ergonomic assessment & functional movement
- Activity pacing and graded exposure to triggering activities
- Acceptance and Commitment Therapy
- Cognitive Behavioural Therapy
- Environment/task adaptation
- Trauma-informed care
Written by Women’s Health Occupational Therapist and Pilates Instructor Carleen Ginter